
Coronavirus: Updates from UW Medicine
Clinical and research perspectives on severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the cause of the Coronavirus Disease 2019 (COVID-19).
April 24
KUOW: Desperate hunt for testing supplies so Washington state may reopen - "To actually just find supply of these swab kits has not been easy," said Keith Jerome, head of the UW Virology Lab. "Our department chair actually spent days on the phone talking with manufacturers in China, trying to find a connection, and ultimately did."
April 23
ABC News: In scramble for ]test kits, some go to extremes - University of Washington pathologist Geoff Baird was so determined to stock up on COVID-19 test kits for his community that he tapped his department’s reserve funds and teamed up with a businesswoman who worked her connections to Chinese manufacturing plants.
Seattle Met: How Seattle Copes: Estela Tabangcura keeps patients rooms clean - Every morning, custodian Estela Tabangcura applies her armor: gears up—gloves, mask, eye shield. Then she and the rest of the first-shift housekeeping squad at University of Washington Medical Center set off to clean rooms filled with ill patients and contaminated surfaces.
The Associated Press: Nursing homes get tests - even without cases - “It’s much easier to do contact tracing when you know there’s zero cases, or one or two cases. When you have a facility that has five, 10, 15 cases, it’s incredibly hard to know who came into contact with those people," said Dr. Thuan Ong, a UW Medicine geriatrician.
People: How the oronavirus complicates births for moms, babies: “In the last six weeks, our entire world that was known as being normal has completely turned around,” said Dr. Edith Cheng, division chief for maternal fetal medicine at the University of Washington.
The (UW) Daily: UW contributes to relief effort by 3D printing face shields - As the number of patients coming into UW Medicine continues to increase amid the COVID-19 pandemic, there has been a high demand for personal protective equipment. 3D printing communities on and off campus have responded by producing face shields designed for healthcare workers.
April 22
KNKX-Radio: Learning as we go -"The rooms are very quiet, especially for patients who are on a ventilator and sedated and unable to speak," says Basak Coruh, a pulmonary and critical care specialist at a UW Medical Center.
April 21
Reuters: Portraits of caregivers: Reuters photographer David Ryder made time to take pictures of front-line caregivers and staff at Harborview Medical Center and UW Medical Center (Northwest and Montlake campuses).
Seattle Times: Harborview chaplain helps patients, families process coronavirus grief - At 26, and just 18 months out of graduate school, Carly Misenheimer is diving into the deep end of daily life at the hospital, tending to the sick and dying and their families during the coronavirus pandemic.
April 20
Everett Herald: How will it end? Testing, tracing and time - Dr. Geoff Baird outlines the next steps forward amid the pandemic: Test many people for the virus. Isolate those who test positive. Find out who they’ve had contact with. Quarantine them, too, until they can be tested. And repeat until the virus has been stamped out for good.
Seattle Times: How to deliver a baby during a pandemic? It’s a delicate balancing act between staving off the virus and ensuring that patients giving birth can have as “normal” an experience as possible. “the only antidote to this virus is actually no exposure," says Dr. Edith Cheng, a UW Medicine obstetrician.
KUOW: Coronavirus antibody tests will soon be available to Washingtonians - The University of Washington's Virology Lab announced it has begun performing tests that detect whether a person has previously been infected with the 2019 novel coronavirus.
April 17
NPR: The view from a Seattle emergency room as COVID-19 cases level off - Dr. Sachita Shah of Seattle's Harborview Medical Center updates NPR's Ari Shapiro about how her hospital is dealing with the COVID-19 outbreak.
NBC News: Doctors forced to learn lessons on the fly - Dr. Chloe Bryson-Cahn, who works at the Harborview Medical Center in Seattle, where the coronavirus was first reported in the United States, said that “initially it felt like juggling a ton of different things. How are we going to safely get people into the hospital? How are we going to operationalize testing? Who are we going to test?” she said.
tctMD: Could robotic PCI play protective role in pandemics? William Lombardi (Heart Institute at UW Medical Center—Montlake) said his team has continued to perform robotic-assisted PCIs during the COVID-19 pandemic, and said there is potential to reduce exposure by minimizing the number of people and shortening the time spent in the cath lab.
KUOW: Covid-19 immunity permits for Washingtonians? "We do think that having immunity to the virus may be protective," said infectious-diseases specialist Helen Chu. "[But] we don't actually know what the immune signature of recovery is."
Everyday Health: Fear of COVID-19 linked to people delaying care for heart attack - “The number of people who would have routinely come in for heart attacks has dwindled,” says Ravi Hira, MD, an interventional cardiologist with UW Medicine in Seattle.
New York Times: When Duty Calls, and Menaces - “The No. 1 rule is: You don’t create two victims,” said Dr. Douglas Diekema of the University of Washington, who argued that the continuing shortage of adequate protective gear somewhat lessened the moral obligation for health care workers.
CNN: Is it time to reopen? Experts say not quite yet. - Before we start rolling back social-distancing protections, the United States needs widespread, insurance-agnostic public testing and public health contact tracing, Dr. John Lynch tells Anderson Cooper.
Seattle Times: Video vignette with Harborview nurse manager - "This is a new disease; we're learning as we go, but we're committed to taking good care of people," says Carrie Ferrulli, nurse manager on the COVID-19 intensive-care unit at Harborview Medical Center in Seattle.
Spokesman-Review: Pandemic forces medical schools to adapt to virtual learning - First-year medical student Dana Arenz usually spends one day a week interacting with Spokane patients. Now, she’s all online from her South Hill residence to learn through the University of Washington School of Medicine.
USA Today: Baby formula shortages easing after coronavirus panic buying - Avoid almond milk, condensed milk or other milk substitutes that are too low in protein, vitamins and minerals, Chung says. Never give your baby water or juice, Dr. Esther Chung, professor of pediatrics at the University of Washington School of Medicine.
MSNBC: States, business leaders call for mass testing before reopening - Private labs say the demand for coronavirus tests is down and they can now begin testing more patients with less serious symptoms. Dr. Vin Gupta, a UW Medicine pulmonary specialist, sees a problem with that idea.
April 15
McClatchy News: How many coronavirus patients on ventilators survive? - “The simple fact that you’re put on a ventilator does not mean that your outcome is going to be universally poor. What the ventilator does is buy ... the lungs time to recover," said Andrew Luks, a pulmonary and critical care physician.
Today (NBC): One man's recovery offers hope - "For him to get better really gave us some hope," said Dr. Maggie Green of patient Raymond Sismaet, who was on a ventilator for 18 days.
KING-5 News: Volunteers deliver over 50,000 masks to UW Medical Center - A gift donated by the Guardians of the Angeles Foundation will help keep UW Medicine clinicians and patients safe.
Seattle Met: Seattle Is now a city of masks - Do face coverings actually help us? The answer is definitively yes, according to Dr. Paul Pottinger, the director of the Infectious Diseases and Tropical Medicine Clinic at UW Medical Center.
MSNBC: In freezing funds, Trump accuses WHO of litany of coronavirus failures - "We didn't act on the guidance that [the World Health Organization] provided," Dr. Vin Gupta said of the United States presidential admininstration.
April 13
Seattle Times: Can blood from coronavirus survivors cure others? Seattle hospitals to try experimental treatment - Locally, almost a thousand people responded to a call for donors, though most haven’t been symptom-free long enough yet to qualify, said Dr. Anna Wald, an infectious disease specialist at the University of Washington.
GeekWire: UW Medicine begins coronavirus testing for all patients admitted to its hospitals - “We are finding people who are asymptomatic who have COVID in their nasopharynx when we swab them,” said Chloe Bryson-Cahn, an assistant professor of medicine at the University of Washington School of Medicine.
KOMO News: UW Medicine sheds light on ventilators as a key to surviving COVID-19 - “When we extubated the first patient that I took care of that was critically ill on a ventilator and he took a sip of a Mr. Pib, he drank that soda like it was the last soda on earth,” said Dr. Vikram Padmanabhan.
New York Times: Hospital chaplains try to keep the faith during pandemic - “We are walking in the valley of the shadow of death, along with our patients and their families,” said the Rev. Katherine GrayBuck, a chaplain at Harborview Medical Center in Seattle. “My work usually brings me close to the end of life, and to death, but this is a whole new era.”
Washington Post (video): With coronavirus victims dying alone, doctors and families share a common grief - "I've seen more crying doctors and nurses in the last two weeks than I remember in my career because of the stress ... of watching families have to be at a distance and patients being alone," said Dr. Randy Curtis, a pulmonary care expert at Harborview Medical Center.
KNKX: The virus-eye view - How does the coronavirus make us sick? We follow the virus as it enters the body, and get the blow-by-blow as it goes about its dastardly business of locking on to a cell, invading it, taking over its machinery and turning it into a virus factory. UW Medicine scientists Lexi Walls and Wes Van Voorhis provide context.
Seattle Times: How UW Medicine, small business and Amazon combined to airlift testing kits - Using his keys, Geoff Baird attacked a box that had just come from China to the parking lot at a UW Medicine office. Baird, who manages UW Medicine’s laboratories, ripped greedily into the cardboard. “Tubes and swabs!” he called out.
KUOW: Coronavirus surges across nursing homes as facilities plead for tests - “As medical practitioners, we are standing ready to do as many tests as we possibly can,” said University of Washington infectious disease specialist Alison Roxby. “I would love to do that ... but at this time, we are limited by this critical resource that we don't have enough of.”
KUOW: How Covid-19 is complicating CPR for some patients - Erin Kross is a critical care and pulmonary care doctor at Harborview Medical Center. She said they talk to patients and families about what resuscitation looks like and what the outcomes might be so people can make informed decisions.
April 9
ABC8 News (Lincoln, Nebraska): Former Husker tackling COVID-19 as surgical resident - Former college football player Sean Fisher is a plastic and reconstructive surgical resident at the University of Washington Medical Center in Seattle, helping with the fight against the coronavirus pandemic.
Washington Post: How a surge of coronavirus patients could stretch hospital resources in your area - “Our hospital was running at over 100 percent capacity all the time, pretty much before this happened,” said Dr. Nick Johnson in the ED at Harborview Medical Center. “And we’ve done a lot of things really early and aggressively to cancel elective surgeries and to try to free up space. But the system’s already pretty taxed.”
CNN: US coronavirus predictions are shifting. Here's why - CNN posed questions to Dr. Gregory Roth, senior faculty at the University of Washington's Institute for Health Metrics and Evaluation, about the new modeling.
Wall Street Journal: In Washington, why the predicted coronavirus surge hasn’t hit - In Washington, why the predicted coronavirus surge hasn't hit - When coronavirus cases began mounting in Seattle in early March, Lisa Brandenburg, president of UW Medicine’s hospitals and clinics, asked a colleague for projections on how many more patients she should plan for. His estimate came in several days later: More than 900 in a health system whose roughly 1,550 beds were almost always full.
April 8
NPR: How Safe Is It To Eat Takeout? - "There are no published reports of linkage to food [of the novel coronavirus]," says Dr. Rachel Bender Ignacio, an associate professor of allergy and infectious diseases at the University of Washington School of Medicine.
Geekwire: How AI is helping scientists in the fight against COVID-19 - Artificial intelligence is playing a part in each stage of the COVID-19 pandemic, from predicting the spread of the novel coronavirus to powering robots that can replace humans in hospital wards. Microbiologist David Baker is interviewed.
Christian Science Monitor: ‘The doctor won’t see you now.’ Rethinking health care delivery in a crisis - Health care workers were already in short supply in many rich countries. But the coronavirus pandemic may yield new approaches to telemedicine and staff recruitment.
April 7
NPR: People connect over coronavirus - NPR's David Green connects Drs. Zachary Levy and Nick Johnson, emergency physicians working with COVID-19 patients on opposite sides of the country, to connect about their experiences.
April 6
KUOW: Are we past the worst of it? A lot of the generalizations that came out in the early days of the novel coronavirus have proven false. Nowhere is that more clearly illustrated by a surprising study of 24 critically ill COVID-19 patients. Pavan Bhatraju is a pulmonary and critical care physician at the UW School of Medicine, and the study’s lead author.
New York Times: Op-ed: Alexa, Do I Have Coronavirus? - Smart devices are equipped to perform passive sensing. For example, instead of “Alexa” or “Hey Siri,” a smartphone, smart speaker or watch could use an on-device “wake word” that is the sound of a dry cough — one of the most common presenting symptoms of Covid-19 infection.
HealthCentral: Could COVID-19 cause a drug shortage? - “People are looking ahead, counting the number of pills, and realizing they’re going to be due for a refill, and not sure if they’re going to be able to get it," says Erika Noss, a rheumatologist at the University of Washington Medical Center.
KNKX: Hospitals try to preserve protective gear as front-line workers brace for 'surge' - "We've been following reports of our fellow health care providers — paramedics, nurses, physicians — becoming infected, dying," said Jamie Shandro, an emergency room doctor at Harborview Medical Center who teaches at the University of Washington School of Medicine. "This shakes all of us."
April 3
CNN: Coronavirus first ravaged parts of Washington state. There are signs of change - "This whole unit was supposed to be for people with brain injuries and strokes and so forth," said Dr. John Lynch, Harborview/UW medicine director of infectious disease control. "So, we had to move all them someplace else because we have to continue that care."
Seattle Times op-ed: With lives on the line, cancer-care specialists battle coronavirus, too - For people with cancer, dealing with their personal health crisis is much more difficult when the entire world is dealing with a global health crisis. That’s why it is so important for healthy people to stay at home so as not to endanger the health of people who are older and/or have underlying diseases.
KREM: UW study finds 50% death rate among critically ill coronavirus patients - Dr. Pavan Bhatraju, the study's lead author, said patients who had to use a ventilator to help them breathe spent an average of 10 days on the machine, longer than ICU patients with other common respiratory problems.
KING-5 News: Real time updates - Certain models of the coronavirus progression estimate that UW Medicine clinicians may have to care for up to 750 more patients at its hospitals in the coming weeks.
IEEE Spectrum: How do coronavirus tests work? - Polymerase chain reaction is the gold standard in viral diagnostics. “Because the sensitivity is so good, it should be the best mechanism for picking up copies of the virus at very early stages of infections,” says Paul Yager, a bioengineer at the University of Washington. “Even if someone is asymptomatic—not yet showing fever or cough—you might very well still pick up a positive.”
April 2
Washington Post: Caring for coronavirus patients in a Seattle ICU: ‘move forward and accept the risk’ - Andy Luks is a pulmonary critical care physician at Harborview Medical Center, which has seen a steady increase in COVID-19 patients. He talks about the challenges of treating these patients and his anxiety about what's to come.
Business Insider: Hospitals deciding how to ration ventilators - "The [pandemic] models only give you a range. And the range goes from very, very bad to just pretty bad," said Mark Tonelli, a pulmonary and critical care specialist and bioethicist at UW Medicine in Seattle. "We're preparing for every eventuality."
NPR: Think you have COVID-19? Here's when to seek help - Anyone who is worried should call their doctor rather than visit. "We're doing a lot more telehealth medicine," says Pavan Bhatraju, an assistant professor of medicine at the UW School of Medince. "Patients should use that as a resource."
April 1
New England Journal of Medicine: How Washington’s Health Care Workers Have Risen to the Pandemic Challenge - As Jennelle Badulak, a UW Medicine intensivist who has helped lead her institution’s response, told me, “In a time of fear and uncertainty, the best thing to have is a protocol.”
Becker's Hospital Review: How 5 hospital pharmacies have responded to the pandemic - UW Medical Center pharmacists are making their own hand sanitizer to supplement their supply, according to Director of Pharmacy Michael Alwan. They're distributing the hand sanitizer to all departments in the health system but are prioritizing it for patient care areas.
Seattle Times: Senior care facilities 'flying in the dark' against coronavirus - The Ida Culver House in Seattle’s Ravenna neighborhood partnered with the UW Medicine after one resident died and another tested positive. The UW found additional cases: three of the 79 residents tested and two of the 67 employees tested were positive, despite the facility not noticing symptoms.
NPR: Why lupus patients find hydroxychloroquine in short supply - Dr. Ruanne Barnabas wants to enroll 2,000 people who will receive the drug after they've been exposed to the COVID-19 virus, to see if it will protect them from getting sick.
Kaiser Health News: Blood centers will collect plasma from COVID-19 survivors in bid for treatment - Seattle-area blood center Bloodworks Northwest is working with the National Institutes of Health and the University of Washington to begin collecting plasma from patients who have recovered from COVID-19. Those donations will become part of a research study co-led by Dr. Terry Gernsheimer, a professor of medicine at the UW School of Medicine.
March 31
KIRO-TV News: Researchers looking for COVID-19 survivors to donate plasma - A team with the University of Washington’s School of Medicine is working with Bloodworks Northwest to recruit COVID-19 patients who’ve recovered to see if the antibodies in survivors’ blood could be a key to fighting the disease.
PBS: For healthcare workers fighting COVID-19, crisis spurred innovation - “We’ve gone from essentially testing only people who were the sickest patients or somebody who had no contact or travel to China,” said Seth Cohen, a physician at the UW Medical Center. “Now, we’re essentially testing most people who are coming in with respiratory symptoms.”
Seattle Times: Coronavirus challenges those trained to help the dying - While losing a loved one to a sudden illness is hard enough, having someone die in the hospital from COVID-19 adds insult to an already unbearable injury. “It’s a double, even a triple whammy,” said Dr. Fred Buckner, an infectious-disease specialist who has been treating COVID patients at the University of Washington Medical Center.
CNN: Inside a Washington hospital preparing for a surge of coronavirus patients: "It's changed how Harborview runs," Dr. John Lynch says of COVID-19. CNN takes its cameras inside the medical center.
USA Today: 6 feet enough for social distancing? - “For me, the question is not how far the germs can travel, but how far can they travel before they’re no longer a threat. The smaller the germ particles, the lower the risk that they might infect somebody who would breathe them in or get them stuck in their nose or their mouth,” said Dr. Paul Pottinger, an infectious disease professor at the University of Washington School of Medicine.
U.S. News: Coronavirus recovery: what to know - For people who aren't sick enough to be in the hospital, recovery is not dramatically different than what's typically experienced with the flu, says Dr. J. Randall Curtis, a UW Medicine specialist in pulmonary, critical care and sleep medicine. "It may take a few days or a week before people feel back to themselves, and a cough may linger."
March 30
KUOW: Seattle researchers to study malaria drug treatment of coronavirus - "We currently don’t know if hydroxychloroquine works, but we will learn in as short a timeframe as possible what the outcome is,” said principal investigator Ruanne Barnabas.
KCPQ-TV: UW Medicine double-study looking at answers for COVID-19 - Two studies are underway and being led by Dr. Helen Chu, an infectious disease expert. The first study will research the effects of an experimental drug called Remdesivir. "It’s an experimental antiviral that has been used in the past for other viral infections. It’s been tried in China and now we’re doing the clinical trial here in the U.S. to see if it may help," said Chu.
Prevention: Life in a Seattle emergency department during COVID-19 - I am a 36-year-old emergency medicine and critical care doctor who works with some of the sickest patients in Seattle, at Harborview Medical Center, a Level I trauma hospital. I was around during H1N1, Ebola, and year-round infection control and disease tracking. But COVID-19 is different because it is a pandemic like we've never seen, and we are one of the epicenters, wrote Dr. Nick Johnson.
Seattle Times: Seattle scientists fast-track potential treatments for COVID-19 - UW Medicine virologist Helen Chu said she’s been surprised by how many patients are in their 30s, 40s and 50s. “This disease seems to be causing young people to get sick, and to get sick very quickly,” she said.
March 28-29
Seattle Times: Coming out of retirement during coronavirus pandemic, a Seattle nurse finds purpose - Carolyn Grant, 63, a registered nurse who had retired from UW Medicine, was sitting in her favorite chair beside the fireplace when her phone buzzed on March 11 with a text message: Could she come back to work?
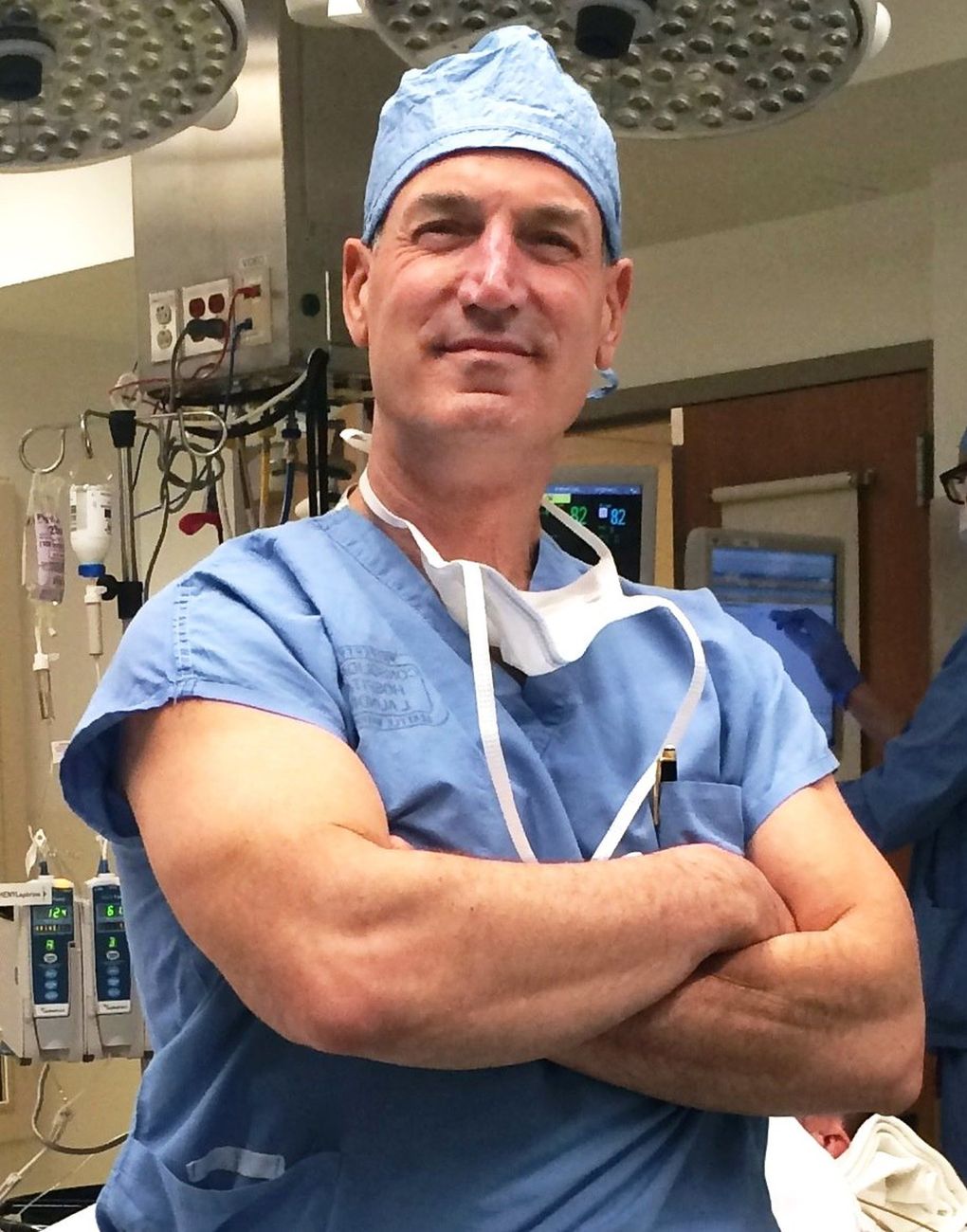
Seattle Times: With surgeries delayed, patients wait with anxiety - “Ee might get to a phase two or three weeks from now where … we can only do true emergencies — someone who might die right now,” said Dr. Douglas Wood (right), who chairs UW Medicine’s surgery department and helped develop the guidelines for the American College of Surgeons.
March 27
Puget Sound Business Journal: THE COVID-19 STRESS TEST - “If you were to try to start today what we did at the beginning, you can’t do it because you simply cannot purchase those things anymore. They’re all gone.” — Dr. Geoff Baird, interim chair of laboratory medicine at the UW School of Medicine
Seattle Weekly: UW doctor offers answers about COVID-19 - “As incredibly boring as staying home can become especially if you’ve got small kids or live alone, it’s absolutely lifesaving for everyone else and yourself.” — Dr. Peter McGough, family physician and medical director of the UW Neighborhood Clinics
TODAY: 'Lab workers are heroes': What it's like to be on front lines of coronavirus testing - "I would say I handle at least 200 specimens during a typical eight-and-a half-hour shift," writes scientist Chris Nelson.
Mail & Guardian (Africa): The coronavirus outbreak through the eyes of a South African doctor in Seattle - With HIV/Aids, there is usually a stepwise progression, even a sense of predictability in the inevitability. With Covid, though, it feels different. Indeed, a few of the older physicians recall this is what it felt like during the first panic-stricken days of HIV in the 1980s. It’s that fear of the unknown.
AAMC: When everything changes: On the front lines of COVID-19 - At UW Medicine in Seattle, an early epicenter of the outbreak, some staff members have been working 20-hour days trying to procure personal protective equipment (PPE) and find ways to make what they have last, such as bundling risky tasks to minimize PPE use.
Seattle Times: UW model says social distancing is starting to work — but still projects 1,400 coronavirus deaths in state - “The trajectory of the pandemic will change — dramatically for the worse — if people ease up on social distancing or relax other precautions," said Dr. Christopher Murray, director of UW's Institute for Health Metrics and Evaluation.
USA Today: Trump says the handshake may not survive coronavirus - “As an infectious disease doctor, I think I speak on behalf of almost all of my colleagues ... when we say, 'Yes, we’ve been worried about handshaking forever,'” said Dr. Paul Pottinger. “This is clearly a great way for people to spread germs, including dangerous germs, from person to person. That’s always been true.”
March 26
Puget Sound Business Journal: UW Medicine CEO says pandemic's financial impact on health care is just beginning - "This is a time for the health care community to come together," said Dr. Paul Ramsey.
WBUR-Radio: What It's Like To Be A Nurse On The Front Lines Of The Coronavirus Pandemic - Mary Jo Kelly and Elizabeth Bridges, two UW Medicine nurses, describe patient care in the era of COVID-19. "I've been a nurse for about 30 years, and this is a very different time than I've seen before," Kelly said.
MedPage Today: Organ Transplant: 'Essential' Surgery in a Time of Pandemic - "There's a reasonable expectation ... in this setting that our organ-transplant patients with their immunosuppression might be at increased risk," both for acquiring the virus and progressing to more severe disease, noted Ajit Limaye, MD, director of the transplant infectious disease program at the University of Washington in Seattle. But that hasn't proved to be true, so far, he said of the program's patients.
TIME: Meet 27 People Bridging Divides Across America - Watching the coronavirus crisis grow, Dr. Paul Ramsey, the CEO of UW Medicine, knew the University of Washington’s virology laboratory was scientifically ready to process COVID-19 tests. What it needed was people. So, on March 13, Ramsey emailed the UW Medicine community asking for volunteers.
Al Jazeera: Our lives after the coronavirus pandemic - "We are in for a revolution in the delivery of primary healthcare. Digital technologies will become even more prominent, and we are likely to see a rise in the use of telemedicine as well as home testing," suggests UW Medicine pulmonologist Vin Gupta.
KIRO7-TV: UW Medicine prepares for patient surge - Harborview Medical Center CEO Paul Hayes says the hospital typically runs at 100% capacity, but is at around 70% now and well-prepared for a surge due to the pandemic.
CBS Morning News: Harborview Hall redesigned for COVID care - The building will be divided into areas to treat homeless patients -- some who are recovering from COVID-19 and, separately, others who have been screened and are awaiting a diagnosis.
March 25
KOMO News: Harborview, UW Medicine to implement coronavirus 'surge plan' - Harborview Medical Center and UW Medicine are gearing up to implement a "surge plan" that will enable its hospitals to better respond to the coronavirus outbreak. The plan is expected to be operational by April 1, said Dr. Steve Mitchell, UW's director of emergency medicine.
NPR: ER Doctor In Seattle On The Challenges Ahead - NPR talks to Dr. Sachita Shah, an emergency physician at Harborview Medical Center in Seattle, about the challenges of the coronavirus response for hospitals and doctors.
Vanity Fair: Experts: Trump’s Touting of an Untested “Game Changer” Coronavirus Drug Is Dangerous - “Trump said it’s a great drug because we know it’s safe,” said Gail A. Van Norman, an M.D. at the University of Washington who has studied the adoption of investigational drugs. “We know nothing of the kind. Claiming that it’s safe for a use for which it hasn’t been tested is a lie.”
Seattle Times: Is 2 weeks enough? Experts say Washington’s ‘stay-at-home’ order may need to continue - “I don’t know of a magic formula for why we’re talking about two weeks,” said Peter Rabinowitz of the University of Washington MetaCenter for Pandemic Disease Preparedness. “It’s a reasonable period for reassessing the impact, but I’m not personally expecting that in two weeks we will be out of the woods.”

Washington Post: Hospitals consider universal do-not-resuscitate orders for coronavirus patients - In Washington state, UW Medicine’s chief medical officer, Tim Dellit, said the decision to send in fewer doctors and nurses to help a coding patient is about “minimizing use of PPE as we go into the surge.” So far, the percentage of infections among those tested is less than in the general population, which, he hopes, means their precautions are working.
Yahoo! News: Nail salons and spas donating masks, gloves to hospitals - In Seattle, one of the hotspots for coronavirus cases, medical spa chain SkinSpirit donated 10,000 gloves, disinfectant spray and wipes to the University of Washington Medical Center.
KOMO-TV: The 90-year-old who beat coronavirus - The times are strange. And all around us there is an air of gloom and melancholy. As an antidote to that, we present the story of Geneva Wood. Covid-19 isn't a death sentence, not even for our senior citizens. Wood received lifesaving treatment at Harborview Medical Center.
BuzzFeed: Her Family Was Careful, And They Got The Coronavirus Anyway - Our family lives in the Seattle area and we’re a white hetero married couple with a number of young children. I am on staff at the University of Washington, which is an important factor in my being tested.
KOMO News: Obstetrician to study COVID-19 impacts on pregnancy - Dr. Kristina Adams Waldorf will move from Zika research to investigating such questions as whether the infection can affect a fetus' growth or placental health and whether this virus heightens the risk for preterm birth or stillbirth.
Seattle Times op-ed: Speaking as a dad and a doctor, we should rethink coronavirus school closures - Dr. Chetan Seshadri writes, "I believe schools can take several steps that will allow our students to continue their education while maintaining equity and relieving the burden on working families."
March 24
Bloomberg News: A Covid-19 Detective Tracks Disease Trail With Genetic Clues - In a few short weeks, Seattle-based biologist Trevor Bedford has emerged as one of the most famous epidemiologists in the world. His frequent tweets are seized upon by many of the globe’s top scientists and health policy makers.
Seattle Met: ‘Immunocompromised’ and the Burden of Chronic Illness During a Pandemic - UW Medicine mentions [as examples of higher-risk circumstances] “cancer, solid organ transplant, other immunosuppressive drugs, chronic lung disease, hemodialysis, advanced HIV.”
MSNBC: Retired health care workers asked to volunteer on front lines - Dr. Ann Marie Kimball, professor emeritus of epidemiology at the UW, is interviewed about shortages in personal protective equipment across the country.
March 23
Pro Publica: The Coronavirus Testing Paradox - Trevor Bedford, a UW Medicine virologist who has been directly involved in detecting and fighting his state’s outbreak, called for a strategy that “revolves around a massive rollout of testing capacity.”
CNN: Is it safe to travel? Avoid it if you can, doctors say - "To 'flatten the curve' people should be staying home, practicing social-distancing and avoiding all nonessential travel," said Dr. Geoffrey Gottlieb, who specializes in infectious diseases at the University of Washington School of Medicine in Seattle.
The Conversation: With every new patient, could this be COVID-19? A Seattle doctor on the frontlines - As emergency and critical care doctors and nurses, we think about and train for these types of situations regularly, but nobody expects to be the epicenter of a pandemic in the U.S. — Nick Johnson, a critical-care physician at Harborview Medical Center
AAMC: Hospitals ramp up telehealth to protect patients and providers - “If you look at what China did, they did a really bad job initially and then it became apparent that they did a lot of things right. One of the things they did right was that they made 50% of their care virtual," says John Scott, medical director for digital health at UW Medicine in Seattle, one of the country’s hardest hit areas.
Brookings Institute: COVID-19’s Painful Lesson in Leadership - Recent articles in GQ, The New York Times, and Kaiser Health News detail how physician-scientists at the University of Washington anticipated the impending crisis, developed a COVID-19 test, and invested millions of dollars to create testing capacity, overcoming bureaucratic inertia at FDA and CDC. By March 13, the University of Washington clinical laboratory had conducted 3 of every 10 COVID-19 tests done in the nation.
GeekWire: Seattle Coronavirus Assessment Network launches - The scientific sleuths who tracked down the origins of the U.S. coronavirus outbreak in the Seattle area have announced a new initiative to crack the case wide-open — and they’re signing up volunteers for self-testing at home. SCAN is an outgrowth of the Seattle Flu Study, which has been using genetic analysis to track the spread of infectious diseases for more than a year.
March 22
Seattle Times: Seattle-area seniors isolate against coronavirus - Seeing even fewer people could compound the feeling of social isolation, said Dr. Richard Veith, a geriatric psychiatrist and former chair of University of Washington School of Medicine’s Psychiatry and Behavioral Sciences department.
Seattle Times: UW researchers look at how coronavirus turns body against itself - “There’s a lot we don’t know [about COVID-19]. We don’t know how it interacts with the cell. We don’t now how it invades it. We don’t know how it overcomes the cell’s innate immune system.” — Michael Gale, a professor of immunology at the UW and the center’s director.
March 21
New York Times: The Hardest Questions Doctors May Face: Who Will Be Saved? Who Won’t? - Dr. Laura Evans moved across the country to direct the intensive care unit at the University of Washington Medical Center in Seattle. The city became one of the first areas in the United States to see community spread of the virus.
Rachel Maddow Show: Panel interview - "Clearly testing is aspirational at this point for the entire country. We know that people who need it don't have access to it. I would say that hope is on the horizon," said pulmonologist Vin Gupta.
March 20
MSNBC: Interview with Dr. Vin Gupta - The pulmonary and critical care physician says a national lockdown is needed to help ensure that doctors and hospitals will not be overwhelmed.
Washington Post: Coronavirus is especially threatening for people with heart disease - The patients who end up dying, says James Town, an intensive care doctor who has been in the thick of it in Seattle, actually die of cardiac rather than respiratory failure.
The American Prospect: The Best Health System to React to COVID-19 - Hugh Foy, professor emeritus of surgery at the University of Washington, agreed. “The VA can react more nimbly now because it’s not profit-driven.”
Mel Magazine: No, the coronavirus has not been in the U.S. for a year - When I put the question to Anna Wald, head of the Allergy and Infectious Diseases Division at the University of Washington — i.e., if someone was sick in November and tested negative for the flu, was that coronavirus? — she emphatically answers, “It wasn’t!”
Business Insider: State labs erroneously told they couldn't use the CDC's coronavirus tests - "In a public-health emergency, it's kind of ironic that all the states had a test that worked. They just didn't have a protocol that worked," Alex Greninger, said assistant director of UW Medicine's Virology Lab.
People magazine: 90-Year-Old Great-Great-Grandma Who Came Close to Dying from Coronavirus Is Now Recovering — Geneva Wood has received her care at Harborview Medical Center.
Seattle Times: We took your coronavirus questions to Seattle’s mayor and two UW experts. Here’s what they said — Dr. Seth Cohen, infectious disease specialist, responds to readers' questions in a virtual panel discussion.
March 19
New York Times: Promising treatment for coronavirus fails - James Town, director of medical intensive care at Harborview Medical Center, said the first choice for most patients would be the remdesivir study. Those not eligible for the study could ask the Food and Drug Administration for "compassionate use" -- special permission to receive an investigational drug outside of a study. Town said the next choice would be hydroxychlorlorine, as long as the patient does had no abnormal heart rhythms, which would make the drug dangerous.
ASBMB Today: 'We are doers. We want to get involved.' - “Something that’s very heartwarming is everybody pulling together within the University of Washington to make this happen,” said John Scott, chair of pharmacology in the School of Medicine. “It started with an idea, and it’s expanded very quickly into action.”
Aunt Minnie: How radiology can get ready for coronavirus crisis - A panel of experts from six institutions has released a list of best practices for radiology preparedness during the coronavirus health crisis. It was published on 16 March in the journal Radiology. The panel includes Dr. Mahmud Mossa-Basha of the University of Washington School of Medicine.
Washington Post: More lifesaving ventilators are available. Hospitals can’t afford them. - J. Randall Curtis, a doctor in Seattle, has treated six coronavirus patients in the intensive care unit at Harborview Medical Center, three of them requiring ventilators (including one who died). He cited as unique in those patients’ care both the intense focus on infection control and also the heavy use of personal protective equipment for medical staff.

Seattle Times: UW pathologist Stephen Schwartz, 78, dies after COVID-19 hospitalization - Stephen Schwartz, pictured at left, a well-known University of Washington pathologist and vocal participant in faculty discussions about university politics, died Tuesday after being hospitalized with COVID-19 infection, the university announced Wednesday. Also: KCPQ-TV, KING5-TV, Inside Higher Ed, The (UW) Daily, TheHuddle, The Scientist
Wall Street Journal: Inside the South Korean Labs Churning Out Coronavirus Tests - Alex Greninger, an assistant director of the University of Washington’s virology division in Seattle, said his team rushed to locate a live virus sample that could prove its test trustworthy enough for FDA standards.
March 18

ABC Nightline: Interview with Dr. Randall Curtis - "It's very unusual for us to keep visitors out and to have these issues around quarantine. That's very hard on the families, obviously, and it's also very hard on the staff."
MedPage Today: COVID-19 Cancels Match Day Celebrations - Sarah Wood, an associate director at the University of Washington School of Medicine in Seattle, one of the areas hardest hit by COVID-19, said administrators there canceled its ceremony on March 6. "Since it was hitting Seattle so early relative to everyone else, I think it's been a lot of navigating things in the dark."
Crosscut: Meet a Seattle scientist racing toward a coronavirus vaccine - If Dr. Deborah Fuller’s moonshot method is successful, she and a team could deliver a coronavirus vaccine months earlier than other methods. Fuller is pictured at right.
Daily Magazine: Coronavirus' risk to pregnant women, newborns seems limited - "The hard part is we just don't have the data, there's only 30-plus cases (known worldwide)," said Dr. Laura Sienas, a UW Medicine maternal and fetal medicine fellow. "In general, pregnant women are at higher risk, but it does not appear to be that much higher risk."
KIRO Radio: UW Virology head details struggle to ramp up coronavirus testing - Dr. Keith Jerome, head of UW Medicine’s Department of Virology, detailed that whereas before, tests were coming back in 8 to 12 hours, backups at labs have had some results taking almost an entire day.
VICE: CDC attempt to make a coronavirus botched basic science - One scientist at the University of Washington, Dr. Helen Chu, had the infrastructure in place to conduct widespread testing in Seattle in the first week February, but was told to stand down by federal regulators.
March 17
NBC News: Household cleaning products can kill the coronavirus - "Bleach is very effective at killing the coronavirus, as well as virtually every other germ on the face of the planet,” said infectious-disease specialist Dr. Paul Pottinger. “The problem is, it’s stinky, it’s hard to use and it can damage what you’re trying to clean.”
KUOW: How we raise the line - To attempt to flatten the viral curve, schools and restaurants are shut down and large gatherings are banned. The other part of the graph is the dotted line that represents the healthcare system's capacity to treat sick patients. Critical care physician Mark Tonelli described how "crisis care" differs from the usual standard of care.
Washington Post video: At the center of the coronavirus outbreak, a hospital prepares for the worst - Dr. Mark Tonelli, a pulmonary and critical care specialist and bioethicist, discusses how UW Medicine is preparing for a surge in cases and what that might mean for patients.
Washington Post: U.S. coronavirus death toll reaches 100 - “I suspect it’s going to be taking off in other locations just like it is in the Seattle area. There’s no reason not to think that. Obviously, that means more deaths,” said Fred Buckner, an attending physician at the University of Washington Medical Center.
March 16
MSNBC: Experts predict shortages in masks, venilators - Dr. Vin Gupta, affiliate assistant professor of health metrics sciences, discusses public health professionals' responses to COVID-19.
MSN: How to properly disinfect your travel gear after a trip - “That’s an easy one,” says Paul Pottinger, an UW Medicine infectious disease specialist in Seattle. “The most important thing to clean after a trip is your hands.”

GQ: Inside the Race to Solve America's Coronavirus Testing Crisis - Laboratory Medicine experts Geoff Baird, pictured at right, and Alex Greninger discuss the struggle to get federal approval for a novel test to diagnose COVID-19.
Forbes: Are Addiction Treatment Facilities Prepared for the Outbreak? - “The DEA needs to approve use of telehealth and phone visits to allow the safe assessment of symptomatic patients by opioid-treatment program providers.” – Dr. James Darnton, general internist at UW Medicine
Slate: We Don't Need a Revolution - Interview with Dr. Fred Buckner about how hospitals are dealing with COVID-19, who is and isn’t being hospitalized, and the important things we need to do during this pandemic. Buckner is a professor of Allergy and Infectious Diseases and Medicine at the UW School of Medicine.
The New Yorker: What went wrong with coronavirus testing in the U.S. - We’ve got a lot of scientists and doctors and laboratory personnel who are incredibly good at making assays. What we’re not so good at is figuring out all the forms and working with the bureaucracy of the federal government,” said UW Medicine virologist Keith Jerome.
NPR: What Is The Treatment For COVID-19 Patients? A Doctor Explains - "We're all preparing for the worst so that we can make sure that we still retain the ability to offer services that we normally offer as well as services for an expected influx of patients. There's a strong esprit de corps at Harborview and at a lot of hospitals like ours where we know that this is our job and we're here to help." – Dr. James Town, UW Medicine specialist in pulmonary, critical care and sleep medicine.
March 15
The Spokesman-Review: Stuck at home? Stay healthy (and isolated) by getting outside - Dr. Darryl Potyk, chief of medical education at the University of Washington School of Medicine and an avid outdoorsman, urged us to forgo the gym and get outside. “Regular exercise can be an important part of our physical and emotional health,” he said. “If at all possible, I would substitute an outdoor workout if you can.”
KOMO-TV: Town hall: COVID-19 Ask the Experts - UW Medicine front-line clinicians and researchers contribute insights. They include Dr. John Lynch, medical director of infection control at Harborview Medical Center; Dr. Peter Rabinowitz, head of the MetaCenter for Pandemic Preparedness and Global Health Security; and Deborah Fuller, a professor of microbiology who is pursuing a coronavirus vaccine.
ABC News: Demand for ventilators spikes as coronavirus looms - "We have a lot of ventilators in reserve," said Dr. J. Randall Curtis, who is on the front lines of the battle against the virus at Harborview Medical Center in Seattle. But he added, “If we hit numbers where all those ventilators are in use … I think we could wind up being in trouble.”
March 13

Wall Street Journal: On the Coronavirus Front Lines in Washington State, Shortages and Delayed Responses - Dr. John Lynch said Harborview Medical Center's infection-control staff has been on call 24/7 for the past three weeks.
Tacoma News-Tribune: UW’s lab needs more pipettes for coronavirus testing - Virology division head Keith Jerome said the shortage is not hindering the lab’s ability to process the current volume.
Reuters: States scramble to slow virus spread, prevent hospital collapse - “Being able to know who has the virus and who does not is able to free up beds, isolation units,” said Alex Greninger, assistant director of UW Medicine Clinical Virology Laboratories, which is testing over 1,000 people a day.
Seattle Times: Virtual-doctor visits help keep patients, hospital staff safe during outbreak - Since confirmed cases of COVID-19 in the region have been climbing and people began dying late last month, UW Medicine has seen a tenfold increase from the 20,000 visits the digital service, which encompasses 20 medical specialties, saw last year, said Dr. John Scott, UW Medicine’s director for digital health.
The Atlantic: The 4 Key Reasons the U.S. Is So Behind on Coronavirus Testing - Former FDA officials I spoke with said that during past outbreaks, EUAs could be granted in just a couple of days. But this time, the requirements for getting an EUA were so complicated that it would have taken weeks to receive one, says Alex Greninger, the assistant director of the virology division at the University of Washington Medical Center, which is located right near the heart of the American outbreak.
Reuters: Drive-through coronavirus tests: coming to a store near you - “There’s really pretty minimal interaction with the patient until you get to the testing step. So it’s really not until you roll down the window and then swab them,” said Dr. Seth Cohen, medical director of infection prevention and employee health at the UW Medical Center – Northwest.
The New York Times: Coronavirus testing goes mobile in Seattle - The UW Medicine’s Medical Center Northwest has turned part of the first floor of their four-story parking garage into a mobile testing clinic. Think fast-food drive-through, but instead of getting served a juicy burger, nurses come to take a nasal swab. “This is a clinic for people who have symptoms,” says Dr. Seth Cohen. At this moment, there is no way for people who are asymptomatic to be screened.
High Country News: Inside a Seattle lab working to develop a COVID-19 vaccine - Science often appears to move at a frustratingly slow rate, especially when something as serious as the coronavirus is spreading so quickly, said Ian Haydon of UW Medicine's Institute of Protein Design. “But science like this needs to move slowly in order to make the proper drugs to save lives.”
March 12

New York Times: Trump and Pence Won’t Be Tested After Meeting With Infected Brazilian Official - “Because of the critical roles that the president and vice president play, it would be wise to have a low threshold for testing regardless of symptom status,” said Dr. Judith Wasserheit, a professor of global health and medicine.
Seattle Times: Coronavirus crisis strains Seattle area’s capacity to deliver care - “Hospitals are being very vigilant. If you have the slightest signs of illness, don’t come to work,” said Alexander Adami, a UW Medicine resident, on Monday.
BBC: Coronavirus: US is failing on testing, says Fauci - "None of us were actually trained in how to deal with the precautions for this disease, or what to do in terms of screening or providing care for these patients," said UW Medicine resident physician Alex Adami.
Reuters: Despite entry of large private labs, coronavirus tests remain scarce in U.S. - One lab at the University of Washington Medical Center ran more than 1,300 tests on Wednesday and may ramp up to 2,300 per day by Friday, said Alex Greninger, assistant director of clinical virology laboratories. “We’re doing one specimen a minute and need to get down to one every five seconds,” he said.
Healthcare IT News: UW Medicine CIO's advice: prepping IT systems for COVID-19 - "Unlike a weather event or a shooting, our response to COVID-19 is a continuously evolving process that has no endpoint and requires us to adapt by the hour," said Dr. Jane Fellner, a UW Medicine physician who provides clinical guidance for electronic health record changes.
GeekWire: Researcher says more coronavirus testing will help manage outbreak, but travel bans? Not so much - The University of Washington’s Virology Lab is now testing more than 1,000 specimens a day, has enough capacity to do 2,000 to 2,500 specimens, and aims to raise that daily capacity to 5,000.
March 11
BBC World News: Interview with virologist Alex Greninger - "I think [the Europe travel ban announced March 11 by President Trump] will make a small difference. I think it's more remarkable and indicative of how policymakers are starting to think about this. They're really starting to take it extremely seriously," said Greninger.
KOMO Radio: Interview with infectious-disease specialist Peter Rabinowitz - "This is like a natural disaster that's happening in slow motion. This kind of disruption is probably going to be happening for weeks or months," says the specialist in allergy and infectious disease, and epidemiology.
Seattle Times: Op-ed - In triaging coronavirus, prioritize vulnerable, healthcare workers - This epidemic is a chance for Washington state to change an approach that has not worked to one that can truly mitigate the impact of the disease on our citizens. It is also what we must do to alleviate the tremendous strain that will undoubtedly be put on our hospitals and health workers. – co-authors Dr. John Lynch, UW Medicine medical director of Infection Prevention & Control, and Karin Huster, clinical instructor, University of Washington Global Health
March 10

Brian Williams' 11th Hour: Interview with UW Medicine virologist Alex Greninger - UW Medicine virologists processed about 730 coronavirus tests on Monday and more than 900 on Tuesday, said Alex Greninger.
Alaska Airlines blog: You asked, we answered: FAQs amid coronavirus uncertainty - "It may be possible that a person can get COVID-19 by touching a surface or object that has the virus on it and then touching their own mouth, nose, or possibly their eyes, but this is not thought to be the main way the virus spreads. The virus is fragile and does not live long on surfaces." – Dr. John Lynch, medical director of Infection Prevention & Control for UW Medicine
New York Times: How Delays in Testing Set Back the U.S. Coronavirus Response - Dr. Helen Chu, an infectious disease expert in Seattle, knew that the United States did not have much time. In late January, the first confirmed American case of the coronavirus had landed in her area. Critical questions needed answers: Had the man infected anyone else? Was the deadly virus already lurking in other communities and spreading?
KOMO News: Testing ability for coronavirus rises as private labs join effort - "Now, there’s more testing for healthcare personnel because the idea is that we want them to be able to return to work faster if they don’t have COVID virus," said Dr. Wesley Van Voorhis, an infectious disease expert.
Seattle Times: What life is like for people who choose to self-isolate - “It’s only human to be anxious about this. If you’re vulnerable — elderly, immunocompromised — the anxiety is even more warranted,” he said. “There are things that can drive the anxiety and things that can help the anxiety.” – Dr. Doug Zatzick, a professor of psychiatry and behavioral science.
March 7-9

NPR: Seattle healthcare system offers drive-through coronavirus testing for workers - For now, the drive-through clinic, pictured at right, is limited to UW Medicine's employees. And they need to have a fever, dry cough, or other symptoms of COVID-19, the disease caused by coronavirus. ... "Hello, my name is Jeff," the nurse the driver. "We're going to be doing your swabs today." (Also in Newsweek, Car & Driver, Becker's Hospital Review, KIRO7-TV)
STAT: Synthetic biologists think they can develop a better coronavirus vaccine than nature could - The emerging field of synthetic biology is answering the SOS over Covid-19, aiming to engineer vaccines that overcome these obstacles. “It’s all of us against the bug,” said Neil King of the University of Washington School of Medicine, who has been part of the hunt for a coronavirus vaccine since 2017.

Seattle Times: Seattle area watches warily as coronavirus spreads - Faced with the unknown, it’s easy for people to fall into a cycle of worry and focus on negative outcomes in repetitive “rumination cycles,” said Michele Bedard-Gilligan, an associate professor of Psychiatry and Behavioral Sciences at the University of Washington School of Medicine. She said the antidote, in these cases, is focusing on what you can control and doing something positive to counterbalance the stress.
The Wall Street Journal: Nursing home at center of Washington coronavirus outbreak target of criticism - Stephen Morris, an emergency physician for UW Medicine who visited the nursing home Thursday, said the facility needed more healthcare workers, and he recommended the state provide help.
March 6
New York Times: With test kits in short supply, health officials sound alarms - Dr. Alex Greninger, an assistant professor at the University of Washington Medical Center in Seattle, said the university’s lab had tested about 400 patients since it set up operations earlier this week. The lab can yield results in about eight hours and is testing patients from several hospitals around Washington state. “I’m entirely focused on testing and building out operations that can handle thousands of tests a day,” he said.
Seattle Times: Seattle healthcare providers scramble to ration medical supplies - UW Medicine dropped its level of precaution for healthcare workers interacting with COVID-19 patients, or those suspected of infection, from “airborne precautions,” in which respirators — such as N95 respirators or PAPR system — are required, to “droplet precautions.”
GeekWire: UW Medicine says it has extra capacity for coronavirus tests -
The University of Washington School of Medicine says its virology lab is now capable of performing 1,000 genetic tests for the COVID-19 coronavirus every day — but all that capacity hasn’t yet fully come into play. “We’ve performed a little more than 400 tests to date over this week,” Alex Greninger, assistant director of the lab, said in an email.
March 5
CNBC: Here’s what to do if you are boarding a plane in the age of coronavirus - “I advise people to bring their own germicidal wipes to rub down the high touch surfaces, the armrest, meal tray and the button that makes your seat go back,” said Paul Pottinger, infectious disease specialist at UW Medicine, the health-care system at the University of Washington in Seattle. “It’s also mighty neighborly to offer one of those wipes to the person you’re sitting next to.”
NPR: When coronavirus struck Seattle, this lab was ready - "We've already gone to three shifts. People are going to be here basically all the time," says Dr. Keith Jerome, a professor who runs UW Medicine's Virology Lab.
Seattle Times: Coronavirus: what’s safe, what’s not — and how to protect yourself and others - The story quotes Dr. Santiago Neme: “Do not let fear paralyze you. … We know that there’s a lot of misinformation and we also know that there’s a lot of unnecessary stigma around certain populations, and I would caution folks and remind them that infections don’t have a predilection. They can affect all of us and we’re all equally at risk so let’s not judge.”
KNKX Radio: Coronavirus basics: A medical expert gives us a foundation for understanding - "According to the CDC you need to use alcohol wipes, which are more than 60 percent alcohol. The other kinds of wipes we have are anti-bacterials. If it’s just an anti-bacterial wipe without alcohol it really won’t do any good because this is a virus," says Dr. Ann Marie Kimball, professor emeritus at UW School of Medicine.
KIRO-7: News at Noon - "We have a small victory in that we have this testing available, but it's likely that the local epidemic is growing and we don't know how big it's going to go," says virologist Keith Jerome.

March 4
Virologists discuss lab test to detect virus: In photo at right, Keith Jerome, center left, and Alex Greninger of UW Medicine's Virology Lab answer reporters' questions at a news conference. Video of the Q&A as well as b-roll of virology lab technicians handling patient samples can be downloaded for use on news programs.
Seattle Times: UW Medicine gets green light to test for coronavirus - “This is a respiratory pathogen that seems to cause significant disease. This is one of the most challenging ones I’ve seen in my lifetime. Seattle and the West Coast are the front lines of this virus and we will do whatever we can to protect the rest of the United States.” – Alex Greninger, assistant director of UW Medicine's Virology Lab.
The Atlantic: Here’s Who Should Be Avoiding Crowds Right Now - “There are people who are walking around who must have it, or have had it very recently, or are about to have it,” said Helen Chu, an infectious-disease professor at the University of Washington School of Medicine.
GeekWire: UW Medicine ramps up new coronavirus lab test; Gates Foundation pledges $5M for detection - The University of Washington School of Medicine is moving forward with a new clinical lab test for the COVID-19 coronavirus, and plans to be able to test up to 1,500 samples per day by the end of the week.
KUOW Radio: Perspective from a family physician - "We're moving from the initial phase, which was isolated cases coming in through travel, to community-based spread," said Dr. Peter McGough, medical director for UW's Neighborhood Clinics.
Sound Publishing: COVID: Call before seeing a doctor, especially the elderly, asthmatic - "For people at high risk, if they get a fever, a productive cough, shortness of breath, contacting one of the nurse lines or contacting your provider initially is a good thing,” said Dr. Pete McGough, medical director of UW's Neighborhood Clinics. Be careful about personal contact; people may have to give up on hugging and kissing for a bit, he said.

MedPage Today: On the Ground With COVID-19 in Seattle - "There's the two groups. There's the one group that says. "Well, it's not really that bad ... there's too much hysteria." And then there's the other group that's worried about what's coming: the "pandemic preparedness group." Those are the people who are clearing out the shelves at Costco, sort of getting ready." – infectious-disease specialist Dr. Helen Chu, left.
KIRO7-TV: Evening News: UW Medicine researcher Vin Gupta says: "What I'd challenge people to do is to take a step back ... look past the hysteria and headlines" to consider what we know: "The vast majority of people do just fine."
March 3
UW Medicine: Lab scientists study 2019 novel coronavirus - The lab of virologist Alex Greninger is studying the latest genomic information about this emerging virus and its possible implications.
Univision: Do hand sanitizers, anti-bacterial wipes help avoid COVID-19? - Dr. Santiago Neme, an infectious-disease specialist with UW Medicine, is interviewed.
Seattle Times: What Seattleites should know about travel amid coronavirus outbreak - "This is not a binary situation; travel is not ‘safe’ versus ‘unsafe.’ In making decisions about travel, individuals must weigh risks and benefits of travel for their particular situation,” said Dr. Geoffrey Gottlieb, an infectious-disease specialist.
March 2
NPR Morning Edition: We answer listeners' questions about the coronavirus - "Most of the respiratory viruses and other infections that you pick up while traveling are through touching contaminated surfaces. And then we unconsciously touch our eyes or our nose or our mouth multiple times an hour," infectious-disease specialist Seth Cohen told reporter Allison Aubrey.
KOMO-TV: Interview with Dr. Seth Cohen - "If you have symptoms, call your doctor's office, call your ambulatory care clinic, or call the emergency department if you really think you need that level of care. Otherwise we encourage people to stay home and self-isolate."
Foreign Affairs: What the World Can Learn From China’s Experience With Coronavirus - An op-ed on the issue is co-written by Dr. Vin Gupta, affiliate assistant professor of pulmonary and critical care medicine at the UW School of Medicine.
KOMO-TV: Hand washing tips to avoid transmitting coronavirus and other diseases, Infectious-disease specialist Dr. Paul Pottinger demonstrates proper handwashing technique. "You have to use a little bit of elbow grease. You're trying to strip away that surface of lipids and cells, both bacterial and the dead cells from your skin," he said.
Seattle Times: New coronavirus cases in Western Washington are likely doubling every 6 days, scientist says - Trevor Bedford, a UW epidemiologist and biostatistician, is interviewed.
KUOW-Radio: Answering your questions on the coronavirus - "We are exposed every year to other respiratory viruses and other coronaviruses. There's at least four other types of coronaviruses that have been in the population for many years. It's just they're more mundane," said UW Medicine microbiologist Deborah Fuller.

GeekWire: University of Washington coronavirus puzzle game aims to crowdsource a cure - UW Medicine's Institute for Protein Design has launched a puzzle game that challenges you to build a protein that could stop COVID-19 from attacking human cells.
March 1
Bloomberg News: CDC Teams Race to Catch Up to Spread of Coronavirus in U.S. - Trevor Bedford weighs in on a genomic test conducted on sample taken for the Seattle Flu Study. The result "strongly suggests" that COVID-19 has been undetected in Washington state for six weeks.
New York TImes: Coronavirus May Have Spread in U.S. for Weeks, Gene Sequencing Suggests - The genetic findings suggest that the virus has been spreading through other people in the community for close to six weeks, according to one of the scientists who compared the sequences, said Trevor Bedford, a UW associate professor of epidemiology and biostatistics.
Feb. 28
Newsweek: Coronavirus was identified two months ago—here's what we still don't know - Peter Rabinowitz, director of the University of Washington's Center of One Health research, said it's difficult to determine how someone contracts the virus.
For details about UW Medicine, please visit https://uwmedicine.org/about.