
How and when immune cells form pathogen memories
Infection-fighting blood cells can change course to become long-lived memory cells instead of short-lived killer cells.Media Contact: Leila Gray - 206-475-9809, leilag@uw.edu
Unexpected findings have emerged about how and when certain infection-killing white blood cells decide to form memories about their encounters with a pathogen.
It has been known for decades that these cells can turn themselves into durable memory cells that can survive a long time after an initial infection is cleared. They are prepared to quickly recognize and eliminate future intrusions by the same kind of pathogen.
That is one reason people are resistant to some infectious diseases after exposure to or recovery from the illness. Vaccinations also work this way, by teaching the immune system to spot and attack dangerous viruses, parasites or bacteria.
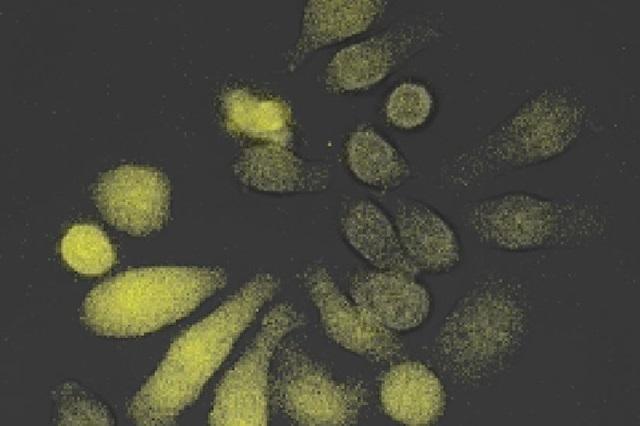
UW Medicine and University of Washington scientists, and their collaborators, wanted to pinpoint exactly when cytotoxic T lymphocytes, a type of immune white blood cell that directly destroys infected cells, decides to form memory during an infection. They used real-time, live imaging to observe these cells over the trajectory of their entire lineage.
Their findings are published Jan. 31 in the journal Immunity from Cell Press. The co-lead authors are Kathleen Abadie and Elisa Clark, both National Science Foundation graduate fellows who recently finished their training in the laboratory of senior author Hao Yuan Kueh, UW associate professor of bioengineering, a joint department in the College of Engineering and the School of Medicine.
“Our experiments revealed an unexpected degree of flexibility in memory decision making, whereby memory T cells are generated at multiple phases during the immune response,” the research team wrote. “After encountering a pathogen, T cells decide early whether to form a memory, or alternatively, to become an effector cell, which has potent cell-killing abilities but is short-lived.”
They added, however, that after the pathogen is eliminated, effector cells can, in essence, change their minds and decide late to join the memory cell pool.
Additionally, the researchers examined the molecular switch that underlies flexible memory formation in these cells. They learned that this switch acts on the key memory regulatory gene Tcf7.
“This switch can turn off Tcf7 early in response to stimulatory signals due to infection,” they explained. “However, importantly, this switch is reversible when these signals are gone, thus enabling cells that have gone down the effector trajectory to reverse their course.”
Why do T cells need leeway in their memory decisions?
“For humans,” Abadie noted, “having some degree of flexibility to change their minds after decisions have been made allows individuals to better adapt to uncertain and changing circumstances.”

The same might be true for T cells to respond effectively to different threats.
An analysis of a mathematical model of T cell decisions, the researchers explained, shows that this flexibility allowed memory to form of both virulent pathogens that demand a large-scale immune response as well as of slow-dividing pathogens that don’t try to overwhelm the immune system, but instead attempt to evade it.
“The ability to make memory fate decisions at multiple junctures during an infection might also allow for greater responsiveness during the evolving situation of an immune challenge,” the researchers added.
These sorts of studies, Abadie and Clark noted, could resolve the longstanding uncertainty surrounding how and when memory cells form.
They hope the findings will open new avenues of research on boosting long-term immune protection against a variety of infectious diseases and cancers.
These studies were performed in collaboration with Jay Shendure, professor of genome sciences at the UW School of Medicine, and Junyue Cao, a former member of his lab, as well as with Armita Nourmohammad, UW associate professor of physics, and Obinna Ukogu, a graduate student in her lab. The Kueh lab team also worked with the lab of Rafi Ahmed at Emory University, together with co-lead author Rajesh Valanparambil, a member of the Ahmed lab.
This study was funded by a National Institutes of Health National Institute of Biomedical Imaging and Bioengineering Trailblazer Awards (R21EB027327), an NIH National Human Genome Research institute grant (R01HG01632-01), National Science Foundation Research Fellowships, an NSF CAREER award (2045054) and startup funds from the Department of Bioengineering and the Department of Physics at the University of Washington, and the Rockefeller University. Shendure is an investigator of the Howard Hughes Medical Institute.
For details about UW Medicine, please visit https://uwmedicine.org/about.
Tags:immunity