
Secret ingredient in new diabetes guideline: patient POV
A UW Medicine patient was integral to generating global recommendations for care involving diabetes and chronic kidney disease.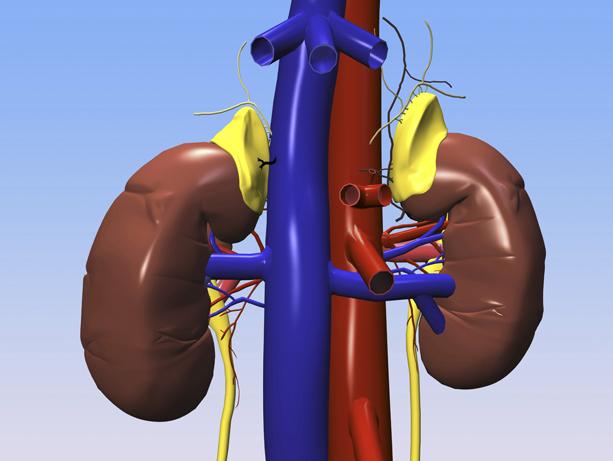
A new treatment guideline published today aims to improve the care of people everywhere who have diabetes and also face chronic kidney disease. This guideline breaks ground with past efforts by incorporating the viewpoints of patients.
“I saw it as a superb opportunity,” said Tami Sadusky, one of two patient contributors. “The guideline is based on research and facts, as it should be, but when you’re developing recommendations for patient care, what a novel idea to have a patient in the room!” she said.
The new recommendations come from Kidney Disease: Improving Global Outcomes (KDIGO), an independent body created in 2003 to develop evidence-based advice for patient care. More than two years ago, KDIGO recruited clinical and research specialists to start poring through study findings that could help people with kidney disease manage diabetes and its complications.
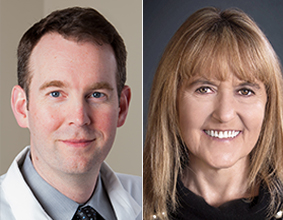
KDIGO’s decision to prioritize non-clinicians' views reflects a widespread effort by healthcare systems to amplify patients’ voices in clinical decisions, said Dr. Ian De Boer, a professor of nephrology at the University of Washington School of Medicine. He co-chaired the writing group for the new guideline.
“Guidelines are often focused on biochemical outcomes and numeric targets that physicians appreciate. This guideline does that quite a bit less than others,” De Boer said. “It really focuses on clinical outcomes relevant to patients rather than intermediate measures like someone’s potassium level or urine albumin concentration.”
Sadusky, 59, was diagnosed with type 1 diabetes at age 13. As her heath steadily declined over a 20-year span, she developed numerous vision- and nerve-related complications of diabetes, and then chronic kidney disease. Ultimately she received a transplanted pancreas and kidneys that saved her life and resolved her diabetes. Today she is a patient advocate on the advisory council for the Kidney Research Institute at the University of Washington.
“In days of old, you’d go to the clinic and the doctor would say, ‘Do these three things,’ and the patient would say ‘OK’ and go home,” Sadusky said. “I think I brought to the (KDIGO) table the idea that the patient needs to be part of the care team’s decisions—for their own well-being. We shouldn’t just leave it to the doctor to anticipate problems that we patients can actively monitor. Physicians need to encourage patients to take an active role in care, to look at blood test results on their electronic health record, know what they mean, and watch for important changes. ”
The guideline authors examined new drugs and technologies as well as behavioral modifications and health systems’ approaches to management. This guideline has global application because the authors considered regulations, populations, and resource constraints that physicians manage in non-U.S. environments.
The presence of chronic kidney disease, or its imminent threat, changes how physicians manage diabetic patients’ medications and goals of care. Confusion exists among clinicians, De Boer said, in large part because kidney disease alters the menu of medications to choose from and how medications should be managed.
“I think the guideline that will get the most attention involves drugs for type 2 diabetes management,” De Boer said. “There’s been an explosion in literature and evidence for SGLT2 inhibitors and GLP1 receptor agonists, and clinicians are wondering how to apply new data. We tried to be very clear about when, and for whom, drugs should be used, based on an excellent base of evidence now available.”
Two others with UW credentials contributed to this KDIGO guideline: Dr. Katherine Tuttle, a UW clinical professor of nephrology, and Katy Wilkens, a dietitian with Northwest Kidney Centers who earned her master’s in Nutrition Sciences from the UW.
For details about UW Medicine, please visit https://uwmedicine.org/about.