
Congenital heart deficit makes patient twice a trailblazer
Her first intervention was at the dawn of open-heart surgery. This month she got a newly available pulmonary valve, placed with a tiny incision.
In 1958, Susie Knudsen became a 12-year-old trailblazer as one of the first children anywhere to undergo open-heart surgery. After she suffered a heart attack in gym class at school, doctors at Baylor University Hospital in Dallas repaired a congenital defect, expanding the pathway through which her heart pushed blood to her lungs.
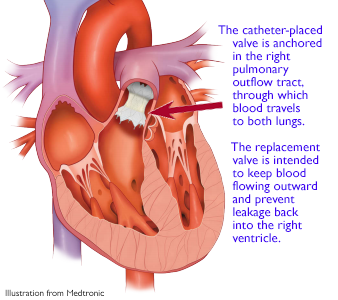
This month, that same heart pathway made Knudsen a pioneer again. No longer benefiting from her surgery of six decades ago, she received a catheter-implanted pulmonary valve on June 11, as UW Medicine cardiologists became first in Washington state to offer the new Medtronic device.
 “I feel very lucky to be the new guinea pig,” said Knudsen, now 76, who lives independently in Lynnwood, just north of Seattle. “I can’t believe I’m not huffing and puffing anymore.”
“I feel very lucky to be the new guinea pig,” said Knudsen, now 76, who lives independently in Lynnwood, just north of Seattle. “I can’t believe I’m not huffing and puffing anymore.”
Pulmonary valves are frequent trouble spots among people born with congenital heart defects, said Zachary Steinberg, Knudsen’s doctor at the UW Medicine’s Heart Institute. “The valves or pathways don’t fully develop or aren’t large enough,” he said, and too little blood flows to the lungs to be oxygenated.
When a baby is found to have such a deficit, surgeons employ work-arounds – patches, conduits and other techniques – because no mechanical valves will fit the heart’s small size and also grow with the child. The work-arounds allow the heart to function, though often not ideally. Such surgeries can result in a leaky pathway whereby blood flows backward into the heart, increasing its workload.
Nonetheless with close monitoring, surgery can get a child to their teenage years, when they can be implanted with a bioprosthetic valve. That valve lasts about a decade before it, too, must be replaced, Steinberg said.
So goes life for many congenital heart defect patients: They face a series of emotionally and physically taxing surgeries.
It’s one reason why cardiologists have been so quick to adopt catheter-delivered devices, which require just one small incision and are guided by wire through blood vessels to an exact position. These nonsurgical procedures dramatically shorten patients’ recoveries, compared with open surgery.
Knudsen was lucky to have a relatively minor congenital deficit: Her right pulmonary outflow tract was too narrow, which surgeons in 1958 resolved by making a cut in her pulmonary valve to let more blood pass through.
This strategy worked for decades, but two years ago her health started to falter. Fatigue came easily and simple conversation left her short of breath. Her right ventricle was enlarged from years of worsening regurgitation – blood flowing backward from the lungs. In late 2020, Knudsen’s community cardiologist referred her to UW Medicine.
Steinberg, along with Drs. Tom Jones and Brian Morray at Seattle Children’s, had recently participated in a clinical trial of Medtronic’s “Harmony” device, a catheter-placed valve that the Food and Drug Administration approved in late March for patients with severe pulmonary regurgitation.
The new Medtronic device will help cardiologists reduce the surgical burden long endured by congenital-heart patients with pulmonary-valve issues, Steinberg said.
“We are not abolishing the need for the original surgical repair for babies with congenital deficits, but for adult patients like Sue Knudsen, surgical valve replacement was the only option until now.” He added that the Harmony valve’s likely recipients will range from teens to senior citizens.
The device spared Knudsen a second surgery, and so far her recovery has been a stark contrast to that of so many years ago.
“In 1958, I went into Baylor in July and came out three months later. I was under such restrictions that I could not go back to school in the fall. … This time, I couldn’t believe how easy it was. I left the hospital after two days, and I think they kept me an extra day because of my age,” Knudsen said. “I was on the treadmill yesterday morning. I feel so thankful.”
###
UW Medicine’s Heart Institute and Seattle Children’s Hospital share a program of care for patients with congenital heart deficits.
– Brian Donohue, bdonohue@uw.edu, 206.543.7856
For details about UW Medicine, please visit https://uwmedicine.org/about.