
Mild COVID-19 elicits persistent immune memory
A study detected a sustained, multipronged arsenal against the pandemic coronavirus in recovered individuals.Media Contact:
- UW Medicine: Leila Gray, 206.475.9809, leilag@uw.edu
- Seattle Children's: Lindsay Kurs, 206.987.5752, Lindsay.Kurs@seattlechildrens.org
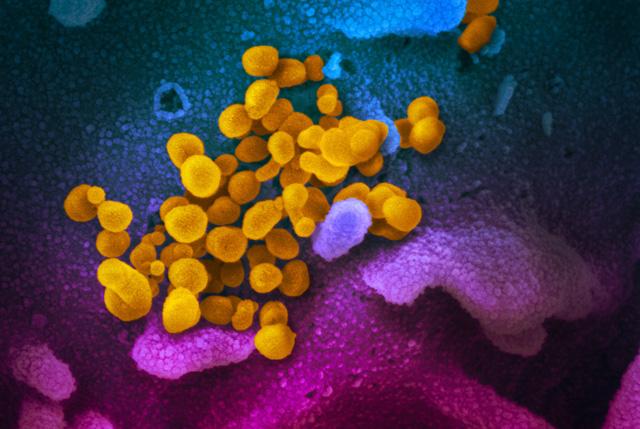
A longitudinal study of mild adult cases of COVID-19 showed that a multi-layered immune memory response, specific to the pandemic coronavirus SARS-CoV-2, could be detected in the study blood for at least three months after illness was over.
In the project’s laboratory experiments, several of these immune-memory defenses displayed powerful attributes associated with antiviral immunity. While the lab findings are promising, the scientists do not yet know if they translate to ease in fending off a re-infection.
The researchers noted, “It is critically important to understand if SARS-CoV-2 infected individuals who recover from mild disease develop functional immune memory cells capable of protecting them from subsequent SARS-CoV-2 infections, thereby reducing transmission and future COVID-19 disease.” Such research could also be useful in assessing vaccination response and duration.
The study was conducted on 15 individuals, median age 47, who had mild symptoms lasting, on average, about 13 days. They entered the study when the inflammation that accompanies acute infection had resolved. Healthy individuals who had no evidence of contracting the virus underwent similar testing as controls.
In most of the subjects, coronavirus-neutralizing antibodies, which are one aspect of this intricate immune response, continued to be detected in the blood for at least three months after recovery – the duration of the study period. It is not yet known what level of antibodies is required to provide protection or if that level can be maintained long term.
The study participants had produced virus-specific memory B and T cells, types of white blood cells that persist as a reminder of successfully overcoming this infection – and possibly as preparedness for any future encounters with the same or similar germs.
Most other infection-fighting cells die during or soon after the battle. In contrast, the memory B cells actually added to their numbers. The memory B cells were capable of producing antibodies that can disarm SARS-CoV-2. In additional lab experiments, the memory cells recognized the coronavirus, or its dangerous apparatus, and commenced antiviral retaliation.
For example, the memory T cells secreted cytokines, chemical signals to other cells for help, upon crossing paths once more with their past nemesis.
The researchers, in their paper, explained the general forces that are hoped might be at work here: Memory white blood cells stay quiet in the body, but are “strategically positioned to rapidly reactivate in response to re-infection” and to execute the defensive programs imprinted on them during the initial infection.
The study results are reported in the journal Cell. The senior authors of the study are Marion Pepper, associate professor, and David J. Rawlings, professor, both in the Department of Immunology at the University of Washington School of Medicine in Seattle. Rawlings is also at the Seattle Children’s Research Institute. The lead authors are Lauren B. Rodda and Jason Netland, both researchers in the Pepper Lab at the UW medical school.
The scientists noted that one of the limitations of their study is its small cohort size. This made it difficult to correlate patient characteristics with maintained immune memory. It also did not cover the disease spectrum from asymptomatic to severe. The short length of this study as well did not allow for determining how long the memory immune response might continue. Subsequent papers, however, have confirmed these results looking several months later.
Continuing research is underway to determine how these immune memory responses might change with time. The scientists also want to learn how the immune system in those who have recovered from mild COVID-19 responds to coronavirus vaccination, compared to those who have not had this infection.
The study reported in Cell was supported by grants from the National
Institutes of Health (NIH2T32 AI06677, R01AI127726, NIH U19AI125378-S1, R01AI150178-01S1, TL1 TR002318), a Research Integration Hub Covid-19 Award, a Bill & Melinda Gates Foundation Grant OPP1156262, a COVID Pilot grant and an Emergent Ventures Fast Grant.
Related:
- Seattle Children's Blog: Study offers good news on COVID-19 immuniity
For details about UW Medicine, please visit https://uwmedicine.org/about.
Tags:immunologyCOVID-19