
Just making genetic tests available is not enough
When a diverse group of patients were invited to take a genetic risk test for common, preventable diseases, only 7% accepted.Media Contact: Leila Gray, 206.475.9809, leilag@uw.edu
Findings from a recent UW Medicine study suggest that a large proportion of people who should receive genetic screening according to published guidelines are being missed.
About one to two out of a hundred Americans carry a harmful genetic mutation that increases their risk of developing cancer or cardiovascular disease. In many cases, the risk could be reduced with lifestyle changes and medical interventions, if started in time.
Yet, despite a large drop in the costs of genetic screening tests that can detect these variant genes, most people do not get tested until they have developed cancer or, in the case of hereditary cardiovascular risk factors, heart and vascular disease. By then, the opportunity to prevent disease has been lost.
Part of the problem is that patients are not routinely screened for these variants unless they have a strong family history of one of these genetically linked diseases. But many patients don’t know if they have a family history of these diseases. Also, most healthcare systems do not systematically collect patients’ family histories in a way that might help identify those who might benefit from testing. Screening rates are particularly low among patients from racial and ethnic minorities.
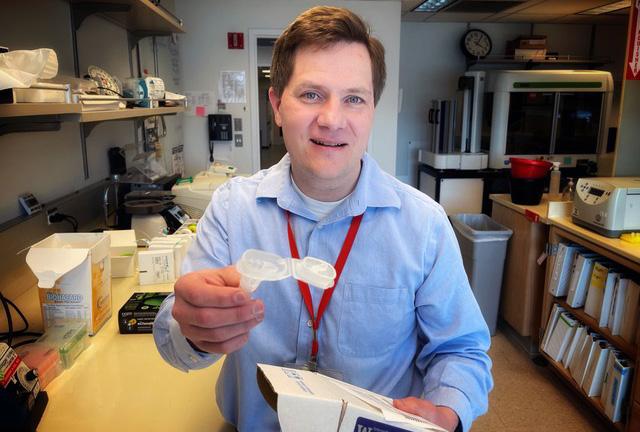
“We have these tests,” said Dr. Brian Shirts, associate professor of laboratory medicine and pathology at the University of Washington School of Medicine, ”but the question is how we can deploy them within our healthcare system in a way that benefits the most people.”
One strategy that has been proposed to increase the number of people being screened is to screen patients without determining if they had risk factors beforehand. To test one such approach, Shirts and his colleagues evaluated a screening program in which patients whose risk was not known were invited by email to be tested. In the study, they looked to see how many of the invited patients participated and how many of those were found to have “actionable” variants, that is variants whose risk could be reduced by lifestyle changes or medical intervention.
The results of the study are published April 18 in the journal Genome Medicine. Nandana D. Rao, a doctoral student in the UW’s Institute for Public Health Genetics, is the paper’s lead author. The paper is titled “Diagnostic yield of genetic screening in a diverse, community-ascertained cohort.”
To recruit patients, the researchers sent email invitations to be tested to a racially and ethnically diverse group of more than 40,000 patients who received their care from the University of Washington’s medical system, UW Medicine. It is one of the first studies to use such a test to screen a large population whose gene samples were not already collected and stored in a repository. It was also the first to test over 10 hereditary cancer risk genes.
Patients who enrolled were sent a kit to collect and mail back a sample of their saliva from which their genetic DNA could be extracted. The DNA was then tested with a low-cost assay, developed by the UW team, that identified variants in 25 genes for common, preventable inherited diseases. To assure the participating population was diverse, the invitations to enroll were preferentially sent to patients from racial and ethnic minorities and 1,000 invitations were sent to individuals self-identifying as LGBTQ+.
A total of 2,889 patients, or 7% of those invited, enrolled. Many invitees did not click on the invitation to enroll, others viewed the email but did not complete the enrollment process, and others enrolled but failed to return the saliva sample kit. Black men were the least likely to enroll. Native Americans and those who were multiracial or self-identified as “other race” were most likely to drop out. More than half of enrollees had a family history of cancer, 61% had a college or advanced degree, and 38% reported having a household income greater than $100,000.
Because access and cost were not factors, distrust of the health system might play a role in the reluctance of people to participate, Shirts said. Patients were often concerned about data privacy, and some were apprehensive about genetic testing in general, he said.
Of the 2,864 enrollees who completed the process and received results, 103 were found to carry at least one genetic variant that could be addressed with preventive measures. It turned out that 31 of the 103 tested knew beforehand that they carried one or more health risk genes.
All told, the screening program identified 74 new patients who carried the risk genes, a diagnostic yield of 2.6% of enrollees who complete the testing. That is about twice the rate seen in studies that looked at at fewer disease risk genes.
About 20% of these patients would have met criteria for screening.
"The findings indicate that low-cost genetic screening can make a difference in communities underrepresented in genetic testing,” Shirts said. “But, like colonoscopy screening and mammograms, which we’ve known are important for a long time, it takes a lot of effort to make sure people are aware of screening tests, have access to them and feel comfortable taking advantage of them. In order to implement genetic screening so that it benefits everyone, it will take a lot of collaborative work.”
The UW School of Medicine’s Brotman Bay Institute for Precision Medicine funded the study.
For details about UW Medicine, please visit https://uwmedicine.org/about.