Gene loss may explain how salmonella causes typhoid fever
Finding may lead to treatments for an infection that sickens 9 million a year and kills 110,000 worldwide.Media Contact: Chris Talbott - 206-543-7129, talbottc@uw.edu
Salmonella is primarily known as a common cause of food poisoning in the United States, which includes the typical symptoms of abdominal pain, cramping and diarrhea.
Some salmonella bacteria, however, can cause a serious, prolonged infection called typhoid fever. While it is uncommon in the United States, typhoid sickens more than 9.2 million people worldwide and kills more than 110,000 annually.
Even with treatment, some people with typhoid will become chronic carriers, shedding bacteria over many years. Salmonella's ability to evade the immune system and cause a chronic typhoid infection has been unclear to doctors and scientists.
A new study suggests that the salmonella variants that cause typhoid acquired this ability by shedding genes responsible for many of the acute symptoms of food poisoning.
The study was conducted by researchers from UW Medicine, Duke University, the University of Massachusetts Medical School and the Jackson Laboratory.
The research is described in a paper published in the journal mBio. The paper's senior author is Dr. Ferric Fang, University of Washington School of Medicine professor of laboratory medicine and pathology and of microbiology. Taylor Stepien, a graduate student in the Fang lab, is the paper’s lead author.
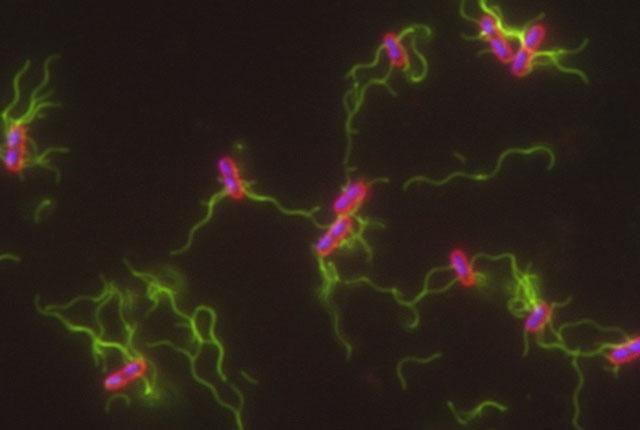
Salmonella variants are classified into groups called serovars. Serovars that cause food poisoning are taken up by cells in the intestinal lining called macrophages. Macrophages are part of the frontline of our immune defenses. They engulf and digest invading pathogens and stimulate other immune cells to respond to the infection.
These food-poisoning serovars, however, have genes that allow them to survive and multiply within macrophages and then cause the macrophages to self-destruct, releasing new bacteria that can go on to infect other cells and be shed into one's stool.
“The basic survival strategy of salmonella that cause normal food poisoning is to grow to high levels in your intestine, trigger a robust inflammatory response and get excreted in the resulting diarrhea so it can be picked up by other people,” Fang said.
The salmonella serovars that cause typhoid — typhi and paratyphi — have adopted a different survival strategy. They infect macrophages and prevent them from self-destructing. This allows them to persist within the macrophages and to travel inside them as the immune cells move throughout the body.
The most famous case of chronic typhoid infection was Mary Mallon, an Irish immigrant cook, who was forcibly quarantined after being implicated in a number of infections in New York in the early 1900s.
“Salmonella typhi and paratyphi are stealth pathogens,” Fang explained. “They don’t stimulate a robust immune response. Instead, they have found a way to persist in macrophages and spread throughout the body, causing an infection in which the bacteria can be shed in the stool for weeks to months and sometimes persistently colonizing people, like Typhoid Mary, who can never get rid of it.”
In their study, Fang and colleagues show that salmonella typhi and paratyphi acquired this ability by shedding 12 genes that ordinarily trigger macrophage death.
Nine of these 12 lost genes produce proteins that target a key cellular protein complex called Nuclear Factor-kappa B (NF-kB). These proteins inactivate NF-kB, which causes macrophages to self-destruct. As a result of the loss of these genes, the vigorous immune response and macrophage destruction seen with salmonella food poisoning does not occur with typhoid infections.
The findings suggest that it may be possible to treat typhoid fever or other chronic infections with drugs that inactivate NF-kB. Drugs that act on NF-kB in this way are already being evaluated to induce cancer cells to self-destruct.
“By inhibiting salmonella typhi and paratyphi’s ability to keep the macrophages alive, it may be possible to convert typhoid fever to regular, old food poisoning where the macrophages die, exposing the bacteria to the host defenses that clear them,” Fang said.
This work was supported by National Institutes of Health grants AI112640, AI007509, AI055396, AI007509, OD0426640, AI132963, OD018259, CA034196 and AI146520.
Written by Michael McCarthy
For details about UW Medicine, please visit https://uwmedicine.org/about.